Each foot, on average, has about 250,000 eccrine sweat glands that produce half a pint of sweat each day. Sweating is a natural and important bodily function. It regulates the body’s temperature by cooling the skin so that it does not overheat. In individuals with hyperhidrosis, the sympathetic nervous system works in "overdrive", producing far more sweat than what is required. People with plantar hyperhidrosis experience an excess amount of sweat on their feet. It is estimated that 2% to 3% of all Americans suffer from some form of hyperhidrosis. This condition is often caused by neurologic, endocrine, infectious, and other systemic disease. Other factors that may trigger the condition are heat and emotions.
People with hyperhidrosis may notice an overabundance of sweat on their feet, along with a strong odor. The feet may also have a wet appearance coupled with infections such as athlete’s foot or toenail fungus. The sweat may even appear in low temperatures, such as during the winter months. People with plantar hyperhidrosis often need to change their socks several times throughout the day.
The specific cause of hyperhidrosis is unknown, and many believe it may be caused by over-activity. However, others believe the condition is genetic. Caffeine and nicotine are known to cause excitement and nervousness which are two emotions that may make the condition worse.
If you are looking to treat your hyperhidrosis the most important thing you should do is wash your feet every day. You may even need to wash your feet twice a day, if necessary. You should also make sure you are wearing the right socks. Wool and cotton socks are both known to be good for ventilation, meaning they allow the feet to breathe. You should avoid socks made from nylon which trap moisture and lead to sogginess. Other common treatment options are over-the-counter antiperspirants that contain a low dose of metal salt. In some cases, prescription strength antiperspirants that contain aluminum chloride hexahydrate may be necessary. In severe cases, surgery may be required.
Untreated hyperhidrosis can easily lead to complications. Some complications that may arise from the disorder include nail infections, warts, and bacterial infections. Consequently, it is important that you seek treatment from your podiatrist if you suspect that you may have plantar hyperhidrosis.

Sweaty feet can be more than just an inconvenience, they can also lead to social embarrassment and discomfort. Medically known as plantar hyperhidrosis, this condition involves excessive sweating of the feet regardless of the temperature or level of physical activity. This occurs due to overactive sweat glands. While it can affect anyone, it is particularly prevalent among teenagers and pregnant women, due to hormonal changes, as well as those who are physically active or stressed. Managing sweaty feet involves maintaining good foot hygiene, such as regular washing and thorough drying of feet. Using antiperspirants specifically designed for feet, wearing socks made from moisture-wicking materials, and choosing shoes made of breathable fabrics can also help control moisture. If these methods do not alleviate the problem, the condition might be considered severe. In such cases, it is suggested that you consult a podiatrist who can provide access to more specialized treatments, such as prescription antiperspirants, iontophoresis, or possibly Botox injections for relief.
If you are suffering from hyperhidrosis contact Brian Shwer, DPM of Southaven Foot Clinic. Our doctor can provide the care you need to attend to all of your foot and ankle needs.
Hyperhidrosis of the Feet
Hyperhidrosis is a rare disorder that can cause people to have excessive sweating of their feet. This can usually occur all on its own without rigorous activity involved. People who suffer from hyperhidrosis may also experience sweaty palms.
Although it is said that sweating is a healthy process meant to cool down the body temperature and to maintain a proper internal temperature, hyperhidrosis may prove to be a huge hindrance on a person’s everyday life.
Plantar hyperhidrosis is considered to be the main form of hyperhidrosis. Secondary hyperhidrosis can refer to sweating that occurs in areas other than the feet or hands and armpits. Often this may be a sign of it being related to another medical condition such as menopause, hyperthyroidism and even Parkinson’s disease.
In order to alleviate this condition, it is important to see your doctor so that they may prescribe the necessary medications so that you can begin to live a normal life again. If this is left untreated, it is said that it will persist throughout an individual’s life.
A last resort approach would be surgery, but it is best to speak with your doctor to find out what may be the best treatment for you.
If you have any questions please feel free to contact our office located in Southaven, MS . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Although rheumatoid arthritis attacks multiple bones and joints throughout the entire body, ninety percent of people who actually develop this condition usually do so in the foot or ankle area. Those who develop this kind of arthritis in the feet usually develop symptoms around the toes and forefeet first, before anywhere else. Rheumatoid arthritis appears to have a genetic component. If it runs in the family, then you will be more likely to develop it as well.
Rheumatoid arthritis is an autoimmune disorder in which the body’s own immune system attacks the lining of the membranes surrounding the joints. This causes inflammation of the membrane lining, and the gradual destruction of the joint’s cartilage and even bone.
Some of the most common symptoms that are associated with RA include pain and swelling of the feet. Stiffness in the feet is also another common symptom that people experience. Those who have RA in the feet usually feel the pain in the ball or sole of their feet. This can get to be very painful at times. A person's joints can even shift and become deformed after a period of time.
In order to properly diagnose RA in the feet it is usually necessary for a doctor or podiatrist to evaluate the area. Your doctor will also question you about your medical history, occupation, etc., to determine whether anything in your lifestyle may have triggered the condition. There are a number of tests that may be performed to help diagnose RA, such as a rheumatoid factor test. There is, however, no one single test that will tell you for sure if you have RA. There are different X-rays that can be taken as well to determine if a person has RA in their feet.
There is a range of treatment options for rheumatoid arthritis. Treatment of RA is usually a lifelong process that includes a variety of methods of treatment and therapy. Your doctor can prescribe special shoes that should help with arch support as well as heel support. A physical therapist can help those with this condition learn exercises which will keep their joints flexible. Surgery may be needed to correct some of the issues with the feet, such as bunions, and hammertoes. Fusion is usually the most successful surgical option for rheumatoid arthritis. However, people need to keep in mind that there are some risks associated with these surgeries.
 Rheumatoid arthritis, or RA, is an autoimmune disease that causes inflammation in the joints. In RA, the immune system mistakenly attacks the lining of the joints, causing swelling, pain, and potentially severe joint damage. This can cause problems in any of the 30 foot joints, but it most commonly affects the toes and ankles. RA can also lead to deformities such as bunions, claw toes, or severe flattening of the foot, as well as pain and difficulty walking. Chronic inflammation can weaken the ligaments and tendons in the foot, leading to instability and increased risk of injury. Podiatrists, or foot doctors, can help manage RA-related foot issues by providing targeted treatments. Among them are orthotics to support the joints, advice on proper footwear to reduce stress on the affected areas, and exercises to maintain joint function and mobility. They also monitor for changes or deterioration in foot health that might require more aggressive interventions, including injections or surgery. If you’re a rheumatoid arthritis patient with problems in the feet and ankles, it is suggested that you add a podiatrist to your care team.
Rheumatoid arthritis, or RA, is an autoimmune disease that causes inflammation in the joints. In RA, the immune system mistakenly attacks the lining of the joints, causing swelling, pain, and potentially severe joint damage. This can cause problems in any of the 30 foot joints, but it most commonly affects the toes and ankles. RA can also lead to deformities such as bunions, claw toes, or severe flattening of the foot, as well as pain and difficulty walking. Chronic inflammation can weaken the ligaments and tendons in the foot, leading to instability and increased risk of injury. Podiatrists, or foot doctors, can help manage RA-related foot issues by providing targeted treatments. Among them are orthotics to support the joints, advice on proper footwear to reduce stress on the affected areas, and exercises to maintain joint function and mobility. They also monitor for changes or deterioration in foot health that might require more aggressive interventions, including injections or surgery. If you’re a rheumatoid arthritis patient with problems in the feet and ankles, it is suggested that you add a podiatrist to your care team.
Because RA affects more than just your joints, including the joints in your feet and ankles, it is important to seek early diagnosis from your podiatrist if you feel like the pain in your feet might be caused by RA. For more information, contact Brian Shwer, DPM of Southaven Foot Clinic. Our doctor will assist you with all of your podiatric concerns.
What Is Rheumatoid Arthritis?
Rheumatoid Arthritis (RA) is an autoimmune disorder in which the body’s own immune system attacks the membranes surrounding the joints. Inflammation of the lining and eventually the destruction of the joint’s cartilage and bone occur, causing severe pain and immobility.
Rheumatoid Arthritis of the Feet
Although RA usually attacks multiple bones and joints throughout the entire body, almost 90 percent of cases result in pain in the foot or ankle area.
Symptoms
Diagnosis
Quick diagnosis of RA in the feet is important so that the podiatrist can treat the area effectively. Your doctor will ask you about your medical history, occupation, and lifestyle to determine the origin of the condition. Rheumatoid Factor tests help to determine if someone is affected by the disease.
If you have any questions please feel free to contact our office located in Southaven, MS . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Bunions are large bony bumps at the base of the big toe. Medically known as hallux valgus, a bunion is a misalignment of the metatarsophalangeal joint, or big toe joint. The misalignment will generally worsen with time if left untreated.
The exact cause of bunions is unknown, with genetics seen as a potential cause. High heels and poorly-fitted footwear, rheumatoid arthritis, and heredity all seem to be potential factors behind the exacerbation of bunions. Women have been found to be more likely to develop bunions in comparison to men.
Bunions do not always produce symptoms. The best way to tell is if the big toe is pushing up against the next toe and there is a large protrusion at the base of the big toe. You may or may not feel pain. Redness, swelling, and restricted movement of the big toe may be present as well.
Podiatrists use a variety of methods to diagnose bunions. If there are symptoms present, podiatrists will first consider that it is a bunion. If not, a physical examination will be conducted to check function of the big toe. Finally, an X-ray may be taken to view the extent of the bunion and confirm it is a bunion.
Typically, nonsurgical methods are used to treat bunions, unless the bunion has become too misaligned. Orthotics, icing and resting the foot, roomier and better fitted shoes, taping the foot, and pain medication are usually utilized first. If the bunion doesn’t go away or causes extreme pain, surgery may be required. Surgeons will either remove part of the swollen tissue or bone to straighten the toe out.
If you have a bunion, it is recommended to see a podiatrist. The longer it is left untreated, the worse it may get. Podiatrists can properly diagnose and treat a bunion before it gets worse.
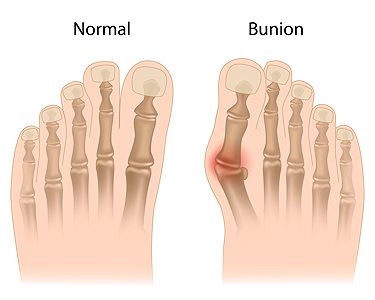
The human foot is a marvel of engineering, composed of an intricate network of bones, tendons, and ligaments that work in tandem to provide stability and mobility. At the center of this complex structure lies the big toe, also known as the hallux, which plays a vital role in maintaining balance and facilitating movement. However, when the alignment of the bones in the big toe is disrupted, a bunion can form at the base of the big toe. This can lead to a further deformity, known as metatarsus primus varus. It results from an abnormal inward angling of the big toe towards the second toe. This misalignment can result in a range of symptoms, including pain, discomfort, and difficulty walking or standing for extended periods of time. While the exact cause of metatarsus primus varus is not fully understood, it is believed to be influenced by both genetic factors and external triggers, such as wearing ill-fitting footwear. People with metatarsus primus varus may experience a variety of symptoms, including pain and discomfort in the foot, restricted range of motion, and skin irritation. Diagnosing metatarsus primus varus typically involves a physical examination and imaging tests such as X-rays. Treatment options may vary depending on the severity of the condition and can include orthotics or surgical intervention to realign the bones and restore normal foot function. For help with managing this deformity, it is suggested that you schedule an appointment with a podiatrist.
If you are suffering from bunion pain, contact Brian Shwer, DPM of Southaven Foot Clinic. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is a Bunion?
Bunions are painful bony bumps that usually develop on the inside of the foot at the joint of the big toe. As the deformity increases over time, it may become painful to walk and wear shoes. Women are more likely to exacerbate existing bunions since they often wear tight, narrow shoes that shift their toes together. Bunion pain can be relieved by wearing wider shoes with enough room for the toes.
Causes
Symptoms
In order to diagnose your bunion, your podiatrist may ask about your medical history, symptoms, and general health. Your doctor might also order an x-ray to take a closer look at your feet. Nonsurgical treatment options include orthotics, padding, icing, changes in footwear, and medication. If nonsurgical treatments don’t alleviate your bunion pain, surgery may be necessary.
If you have any questions, please feel free to contact our office located in Southaven, MS . We offer the newest diagnostic and treatment technologies for all your foot care needs.
The plantar fascia is a connective tissue in the heel that stretches across the bottom length of your foot. Plantar fasciitis occurs when the connective tissue becomes inflamed, causing heel pain and discomfort during physical activity. Although the condition is completely treatable, traditional methods can take up to a year to start becoming effective.
Plantar fasciitis is caused by a number of everyday activities, so understanding the condition is important for managing and treating it. One of the most common causes of plantar fasciitis is excessive running, especially with improper fitting or non-supportive shoes. Too much exercise can lead to the plantar fascia being overworked and overstretched, which can cause tears in the tissue. Along with improper fitting shoes, pronation, the rolling of the feet inward, is a common cause of plantar fasciitis. If not treated properly, the plantar fascia becomes overstretched and starts to tear, causing inflammation.
Despite the common causes of plantar fasciitis, there are many different treatment options. For less severe cases, conservative home remedies include taking anti-inflammatory drugs to alleviate pain, applying ice packs to the bottom of your foot and heel, slowly stretching and exercising your feet to re-strengthen the tissue, and using orthotic devices are all ways to help manage your plantar fasciitis.
For more severe cases, shockwave therapy has become a common solution for plantar fasciitis. Shockwave therapy can effectively break up the tissue on the bottom of your foot which facilitates healing and regeneration. This fights the chronic pain caused by plantar fasciitis. Even if this doesn’t work, surgery is always a final option. Surgery on the tissue itself can be done to permanently correct the issue and stop the inflammation and pain in your heels.
No matter what the case may be, consulting your podiatrist is the first and best step to recovery. Even the slightest amount of heel pain could be the first stage of plantar fasciitis. Untreated symptoms can lead to the tearing and overstretching of tissue. Because the tearing of tissue can be compounded if it remains ignored, it can evolve into a severe case. The solution is early detection and early treatment. Talk to your podiatrist about the possibilities of plantar fasciitis if you’re experiencing heel pain.

Plantar fasciitis occurs when the plantar fascia, a broad ligament that lies under the foot, becomes inflamed due to repetitive stress or strain. The hallmark symptom of plantar fasciitis is sharp, stabbing heel pain that can also radiate along the arch or sole of the foot. It typically worsens in the morning or after prolonged rest but often subsides with movement. Swelling and redness around the heel and arch area may accompany inflammation, and the affected area may feel tender or puffy. Stiffness and tightness in the foot can worsen throughout the day with increased activity. Discomfort in the foot's arch is also a common symptom of plantar fasciitis, limiting mobility and affecting daily activities. Pain and discomfort in the Achilles tendon may result from altered foot movement patterns caused by this condition. If you're experiencing any of these symptoms, it's suggested that you make an appointment with a podiatrist for a thorough evaluation and personalized treatment plan.
Plantar fasciitis is a common foot condition that is often caused by a strain injury. If you are experiencing heel pain or symptoms of plantar fasciitis, contact Brian Shwer, DPM from Southaven Foot Clinic. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is one of the most common causes of heel pain. The plantar fascia is a ligament that connects your heel to the front of your foot. When this ligament becomes inflamed, plantar fasciitis is the result. If you have plantar fasciitis you will have a stabbing pain that usually occurs with your first steps in the morning. As the day progresses and you walk around more, this pain will start to disappear, but it will return after long periods of standing or sitting.
What Causes Plantar Fasciitis?
There are some risk factors that may make you more likely to develop plantar fasciitis compared to others. The condition most commonly affects adults between the ages of 40 and 60. It also tends to affect people who are obese because the extra pounds result in extra stress being placed on the plantar fascia.
Prevention
There are a variety of treatment options available for plantar fasciitis along with the pain that accompanies it. Additionally, physical therapy is a very important component in the treatment process. It is important that you meet with your podiatrist to determine which treatment option is best for you.
If you have any questions, please feel free to contact our office located in Southaven, MS . We offer the newest diagnostic and treatment technologies for all your foot care needs.